You’re sitting in your dermatologist’s office, frustrated and pointing to pale, white-appearing patches on your kid’s skin. “These white spots showed up after I used that steroid cream you prescribed for my eczema!” you say – your voice tinged with worry. You’re upset. Your child’s skin was already a hassle with the itching and redness, and now these light patches make you feel self-conscious. You’re convinced the topical steroids are to blame. But are they? Let’s dive into what’s really going on with post-inflammatory hypopigmentation (PIH) and why your topical eczema treatments are not to blame.
The Clinical Picture: What PIH Look Like
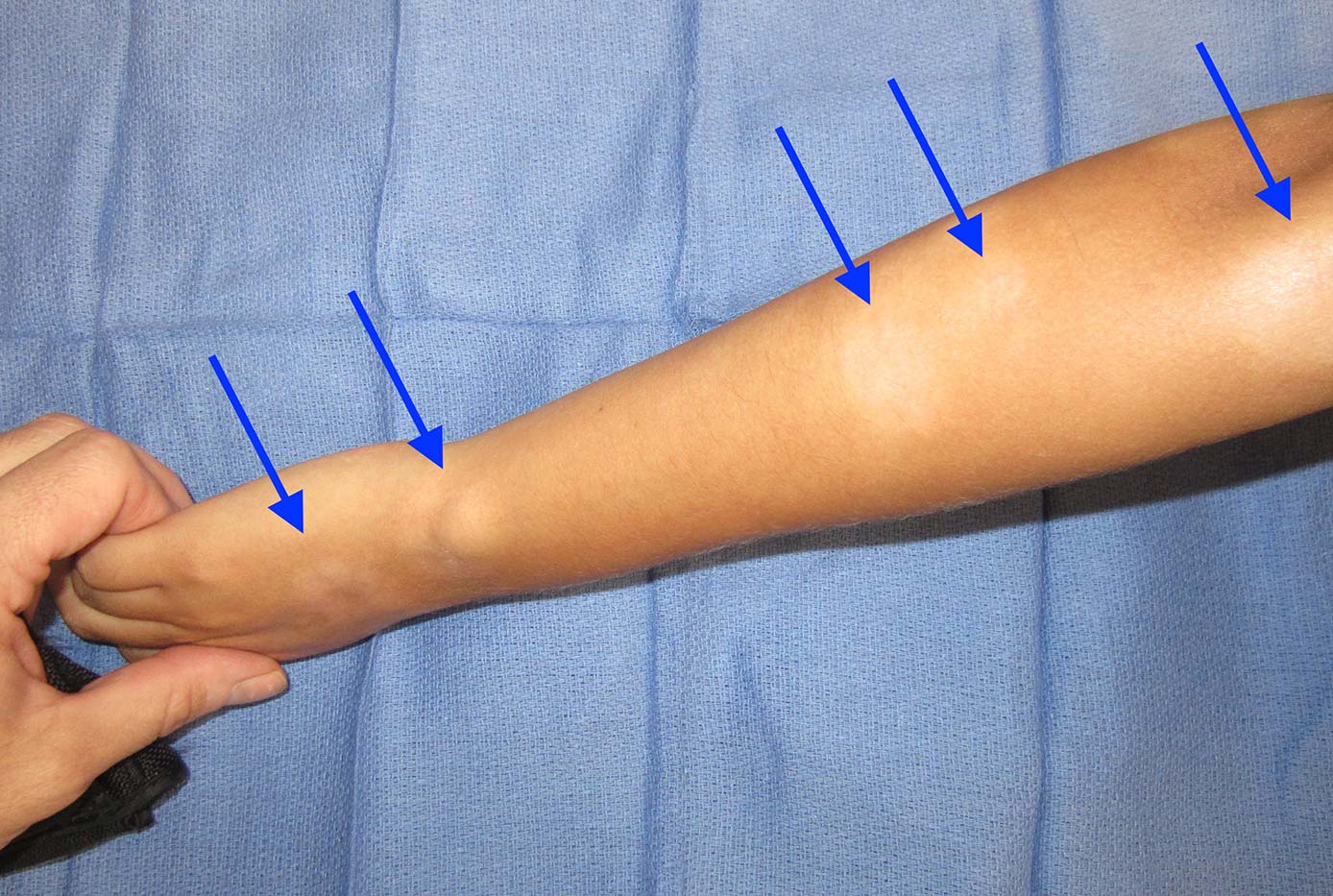
If you or someone you know has eczema, then you might have noticed pale spots where the red, scaly patches of an eczema flare used to be. We call these spots “post-inflammatory hypopigmentation” – or PIH for short. This condition shows up as flat, lighter-than-normal patches on your skin. These patches can be small or large, round or irregular, and they stand out most on darker skin tones, though anyone can get them. They tend to be more noticeable in the summer for reasons that will soon make sense (keep reading!).
They patches do not itch. They do not hurt. They aren’t raised, painful, or itchy—they’re just there, and that’s what drives patients crazy. The frustration is real: you treated one skin problem only to end up with another that affects your confidence. You might even feel betrayed by the treatment, thinking, “I followed the doctor’s orders, and now this?”
The Science Behind PIH: What’s Happening at the Cellular Level
PIH is NOT specific to eczema, and it can be seen after any inflammatory skin condition. For example, psoriasis, acne, heat burns – even a scrape from your new puppy! – can all cause PIH.
To understand why PIH happens, let’s zoom in on your skin cells. Your skin’s color comes from melanin, the tan-colored pigment produced by your cells called melanocytes. When your skin gets inflamed—say, from an eczema or psoriasis flare or a bad acne breakout—it’s like sounding an alarm. Your immune system sends cells to the area to fight the problem, releasing chemicals like cytokines that can disrupt melanocytes. Sometimes, these cells get temporarily “stunned” and stop making melanin. In more severe cases, the inflammation can be severe enough to actually damage or destroy melanocytes, leading to longer-lasting light patches.
In other words, the degree of observed skin lightening depends on how intense and how prolonged the inflammation was. For example, a deep burn or chronic eczema flare-up might cause more noticeable PIH than a mild rash from a quickly resolving virus or a small scrape after some light yardwork.
The one thing all PIH has in common is that it is this cellular disruption – tied to the original underlying cause of inflammation—that causes the white spots to appear. It is NOT the fault or consequence of the treatment used to calm the inflammation.
Do Topical Steroids Cause PIH?
I get asked about 5 times a day in my eczema clinic if the topical steroids I prescribed for my eczema patients, like hydrocortisone (weak) or mometasone (moderate strength) or even clobetasol (super potent), could have caused the PIH. The short answer is, as discussed above, a resounding “NO!” These medications are designed to reduce inflammation. They work by calming the immune response, reducing redness, swelling, and itching. By doing so, they actually help limit the damage to melanocytes that causes PIH.
Think of inflammation as a wildfire in your skin—steroids are like water dousing the flames before they spread further. The light patches you see are a result of the original condition (such as eczema or psoriasis) that caused the inflammation, not the steroid cream used to treat it. However, it’s understandable why you might point the finger at steroids—they’re often applied right before you notice the spots.
But correlation isn’t causation. What’s actually happening, rather, is that the steroids you are applying to the skin are reducing the inflammation and, in turn, calming the eczema flare. Now that you can once again see the “normal” skin that was hiding under the eczema flare it appears lighter and blotchy in term of its tone. You are simply seeing the melanocyte “stunning” effect of the underlying inflammation. Without the steroids, the eczema flare would persist, and the skin underneath would likely get even lighter as time goes by. So, contrary to what many people have posted on the Internet, steroids can make PIH less severe by reducing inflammation faster.
Some of the confusion comes from the fact that misusing steroids (like using a superpotent one like clobetasol for too long) can absolutely cause skin side effects. You may have been specifically warned by your doctor that overusing a steroid can cause “skin thinning” or “atrophy.” This is very different from PIH, and it involves a true thinning of the skin such that you can start to see blood vessels more easily through the affected areas. Thankfully, true steroid-induced atrophy is pretty rare if you follow your doctor’s instructions carefully, and it is usually reversible once the steroid is stopped.
Managing PIH: Practical Steps to Take
The good news? PIH is usually temporary and fades as your melanocytes “snap out of it” and recover their melanin-making function. However, it can take a while to see a full recovery – sometimes even months to years. No one wants to wait that long, so here are some science-backed tips to help minimize and manage PIH and help your skin heal as fast as possible:
- Lighten up: Be patient! Your skin just needs time to regenerate melanin. Rushing to harsh treatments can cause more irritation and inflammation and will only make things worse.
- Gently cleanse, treat inflammation, and moisturize regularly: Hydrated skin heals better. Hydrated skin is less inflamed and less irritated, so hydrated skin is not as prone to PIH. Use a gentle, non-foaming cleanser, an anti-inflammatory, and a fragrance-free moisturizer to support your skin’s barrier. I, of course, am partial to Pediadermics’ Easy as 1-2-3 Eczema Management System!
- Use sunscreen to decrease the contrast with normal skin: Sun exposure can make PIH more noticeable. This is exactly why PIH is usually more evident in the summer and less conspicuous in the winter. The skin under the eczema flare is not making melanin correctly, but the less affected skin around it can still make melanin (i.e., your “tan”). So, now, you start to see the contrast between the two areas, and that usually gets people’s attention. You can help minimize this contrast by applying a broad-spectrum sunscreen with SPF 30 or higher, even indoors or on cloudy days.
- Avoid scratching or picking: Traumatizing the area by scratching (eczema and psoriasis, for example) or picking (acne, for example) can worsen inflammation and delay pigment recovery. Don’t scratch. Don’t pick. Use a topical anti-inflammatory like Pediadermics’ Eczema 2 to help decrease itch.
- Talk to your doctor: If you’re worried about PIH or think your treatment isn’t working, have an open conversation with your board-certified dermatologist. Your board-certified dermatologist can adjust your plan or reassure you about what’s normal. In severe cases, your dermatologist might recommend some additional therapies to help stimulate melanin production in the most severely affected areas, but these are not usually necessary. Always consult a board-certified dermatologist before trying any of these treatments and avoid “online cures” that could make things worse or expose you to something dangerous.
Wrapping Up
If you’re staring at those light patches and blaming your steroid cream, take a deep breath. Post-inflammatory hypopigmentation is a common, usually temporary response to skin inflammation, not a side effect of your topical treatments. Those light spots are your skin’s way of saying, “I’ve been through a lot!” Topical steroids actually help prevent PIH by reducing the inflammation that causes it in the first place. With vigilant care, dutiful sun protection, and a lot of patience, your melanocytes will bounce back, and your skin tone will eventually even out!